Most people have experienced some sort of headache at some point, whether it be in the form of a piercing migraine or a tight tension headache after your computer crashed. Headaches come in all shapes and sizes and from multiple different causes.
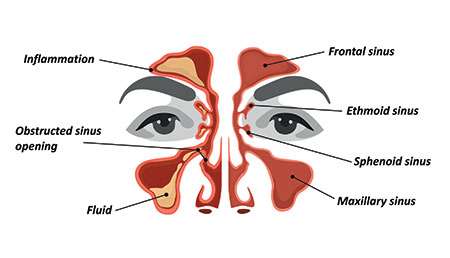 The sinuses of the facial bones are air-filled spaces, with a pair across the forehead and brow (frontal sinuses), two pairs along the bridge of the nose (the ethmoid and sphenoid sinuses), and the largest pair of sinuses across the cheeks (the maxillary sinuses). Sinuses help to retain heat, make the skull lighter, humidify inhaled air, and even help the voice to resonate more loudly. Sinuses can also sometimes be a pain in the neck (or face), particularly when they succumb to allergy or infection. The mucosal lining of these sinuses can become inflamed and swollen and may get a little over-enthusiastic about the production of mucus and pus, which leads to congestion and a build-up of pressure in the affected sinus cavity.
The sinuses of the facial bones are air-filled spaces, with a pair across the forehead and brow (frontal sinuses), two pairs along the bridge of the nose (the ethmoid and sphenoid sinuses), and the largest pair of sinuses across the cheeks (the maxillary sinuses). Sinuses help to retain heat, make the skull lighter, humidify inhaled air, and even help the voice to resonate more loudly. Sinuses can also sometimes be a pain in the neck (or face), particularly when they succumb to allergy or infection. The mucosal lining of these sinuses can become inflamed and swollen and may get a little over-enthusiastic about the production of mucus and pus, which leads to congestion and a build-up of pressure in the affected sinus cavity.
A short foray into the available literature online will tell you that sinus headaches aren’t as straightforward or common as many people think. Studies have found approximately 90% of headaches diagnosed either by a healthcare professional or by self-diagnosis as a sinus headache are in fact migraine headaches.
Rhinosinusitis
Rhinosinusitis is defined as inflammation of the nasal cavity (accounting for the “rhino” part of the word) and the sinuses (this part speaks for itself). Rhinosinusitis itself is not particularly uncommon. The point of contention is whether rhinosinusitis is a primary cause of the elusive “sinus headache.” Some researchers believe that sinusitis, with or without the involvement of the “rhino,” actually is rarely capable of causing a headache or even facial pain. The exception is when the sinus is unable to drain due to an acute bacterial infection and trapped pus within the cavity leads to increased pressure and inflammation.
The majority of acute rhinosinusitis cases (defined as lasting for under 12 weeks) are from a viral infection, rather than bacterial, and only about 2% of viral acute rhinosinusitis episodes transition into bacterial sinus infections. A true bacterial rhinosinusitis is typically preceded by an upper respiratory tract infection for at least 10 to 14 days. Symptoms of acute rhinosinusitis include:
- Nasal congestion
- Runny nose with discolored mucus
- Post nasal drainage
- Cough, usually in children
- Facial or dental pain, usually just on one side of the face
- Facial swelling
- Headache
Specific to a bacterial rhinosinusitis, additional symptoms may also include fever, fatigue, and pressure in the ear.
Viral acute rhinosinusitis episodes usually self-resolve while the majority of patients with bacterial rhinosinusitis will respond readily to appropriate antibiotics such as amoxicillin. Supportive therapy in the form of painkillers, topical steroids and saline irrigation for the nasal passages may also be useful to alleviate symptoms.
Chronic rhinosinusitis occurs with a prevalence of approximately 12% in the US and is diagnosed when symptoms of rhinosinusitis are present for longer than 12 weeks if inflammation of the sinuses can be demonstrated on nasal endoscopy or a CT scan. For those patients who are not adequately responsive to medications such as topical nasal steroids, sinus surgery may be the next option.
If the so-called sinus headache is caused by allergy such as hay fever then a medicated nasal spray containing antihistamines or steroids is the most common treatment. This condition is termed allergic rhinitis and may occur in conjunction with rhinosinusitis though no direct association has been found between the two.
Sinus headaches vs migraine headaches
So, if most apparent “sinus headaches” are in fact migraines, how can one differentiate between the two?
The location of pain is similar between the two conditions, leading many to misdiagnose any pain around a sinus cavity as a sinus headache, but migraine pain can often occur in the same areas. Both sinus and migraine pains are known to worsen when bending forward. For some, migraine headaches may also present with some nasal symptoms, such as a runny nose or pressure around the face. However, the nasal discharge, also known as rhinorrhea, during a migraine is clear and watery whereas in acute bacterial rhinosinusitis you can expect to see a lot more green and yellow lumpy bits. The typical exacerbating factors of a migraine headache are absent in a sinus headache, such as loud noises and bright lights, as are nausea and vomiting. Sinus headaches due to rhinosinusitis tend to last for days or weeks while a migraine headache is expected to resolve within several hours, occasionally lasting up to a day or two.
While primary care physicians are easily accessible and capable of diagnosing a sinus headache from rhinosinusitis, you may be referred to an ENT specialist, particularly if confirmation of the diagnosis is required via a nasal endoscopy or if the condition is complicated and difficult to treat. Accurate diagnosis of the type of headache is important as the treatment is quite different between sinus headaches and migraines. Persistent headaches, especially those unresponsive to over-the-counter painkillers, should be thoroughly assessed by a qualified doctor.
References
Headaches connected to allergies and sinus problems. https://www.aaaai.org/conditions-and-treatments/library/allergy-library/allergy-sinus-headaches
Picture of the sinuses. https://www.webmd.com/allergies/picture-of-the-sinuses#1
What to do about a sinus headache. https://www.medicalnewstoday.com/articles/321012.php
Rhinosinusitis: synopsis. ://www.worldallergy.org/education-and-programs/education/allergic-disease-resource-center/professionals/rhinosinusitis-synopsis
Sinusitis. https://www.racgp.org.au/afp/2016/june/sinusitis/
Sinus headaches: avoiding over- and mis-diagnosis. https://www.tandfonline.com/doi/abs/10.1586/ern.09.8?journalCode=iern20
Sinus headaches. https://www.mayoclinic.org/diseases-conditions/sinus-headaches/symptoms-causes/syc-20377580
