Allergic Rhinitis
How Our Allergy Doctors Treat the Symptoms (and Causes) of Allergic Rhinitis

Allergies are extremely common in the US. In fact, according to the Centers for Disease Control and Prevention, they’re the 6th leading cause of chronic illness.
It is estimated that over 50 million Americans are affected by the symptoms of various allergies. While there isn’t yet a cure for allergies, the good news is that they are manageable and treatable (Asthma and Allergy Foundation of America).
Major allergens include food, mold, pet dander, dust mites, insect venom, latex rubber, medications, and, of course, pollen. Hay fever, triggered by pollen, is one of the most common types of allergies. In 2021, almost 26% of adults (67 million) and 19% of children (14 million) were diagnosed with hay fever (Asthma and Allergy Foundation of America). Hay fever is also referred to as seasonal allergic rhinitis which is an allergic reaction to pollen as well as cat, dog, and rodent dander, dust mites, mold spores, cockroaches, trees, grass, and other environmental allergens. When you have it, you feel like you have a cold. What happens when you breathe in these allergens is that a natural chemical in your body, called histamine, gets released. It’s your body’s natural immune response to these invaders. The downside is that histamine causes the mucus membranes in your nose to inflame. Your nose, eyes, and throat can begin to itch as your body fights to throw the invader allergens out. This is why “anti-histamines” are typically suggested by BergerHenry ENT allergy doctors as an initial option in treating allergies.
Allergy Symptoms
Apart from the itchiness, other symptoms can include nasal congestion, a clear runny or stuffy nose, sneezing, and watery eyes. You can also experience a cough from post nasal drip in addition to loss of smell and taste.
Allergies are typically inherited and thus passed down from family members. So, if one of your parents has had allergies or one of your siblings, aunts, or uncles do, there’s a good chance that you’ll also get allergies.
There are a couple of ways for BergerHenry ENT allergy doctors to diagnose an allergy. They can measure antibodies as they relate to specific allergens with a blood test, also called an immunoglobulin E (IgE) test. You may also be given a skin prick test where different allergens are placed on the skin. It’s a common test that’s painless and accurate but could be just a little uncomfortable. In this instance, your allergy doctor places a small sample of different allergens on your skin (usually on your forearm or back) and scratches or pricks the skin with a needle. Scratching the skin allows the allergen to get under the surface. If redness, itchiness, and irritation occurs within 15-30 minutes, an allergy to a specific allergen exists. You may develop raised, hive-like welts called wheals that indicate that particular allergic reaction.
How Our Allergy Doctors Treat Allergic Rhinitis
The front line treatments for allergies often recommended by BergerHenry ENT allergy doctors are nasal antihistamine sprays and pills, i.e., Flonase, Nasonex, Allegra, Claritin. But, what happens when medicines fail and allergies persist? Moreover, what if you’ve had nasal surgery and still suffer from a stuffy nose, post nasal drip or a runny nose? There’s a possibility that your inferior turbinates (the radiators of the nose) are chronically inflamed (turbinate hypertrophy). If this is diagnosed, we would discuss a treatment that is a highly successful, comfortable, office-based, and minimally-invasive solution called a turbinoplasty. Incidentally, a deviated septum can also cause your inferior turbinates to become inflamed. In this case, a turbinoplasty (turbinate reduction) and septoplasty (straightening of the nasal septum) may be suggested to not only open both of your nasal airways again for better breathing but to also decrease your susceptibility to chronic sinus infections, chronic postnasal drip, headaches, and snoring and sleep apnea.
In-Office Treatment of the Inferior Turbinates
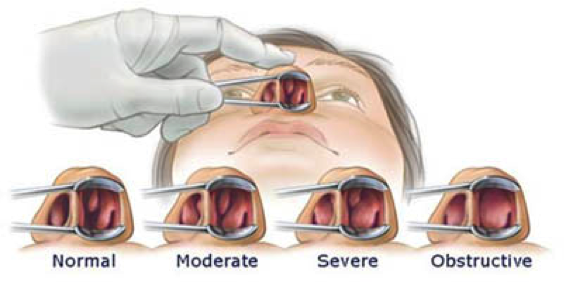
Inside your nose, there are 3 turbinates: the middle, nasal, and inferior turbinates. Think of them as radiators for the nose. Each of them is responsible for conditioning the air that you inhale by humidifying, heating and filtering it. The most important turbinate is the inferior turbinate. Mucous membranes cover the inferior turbinate (and the other turbinates) and can swell or shrink in response to physiological or environmental change (allergies). All individuals have turbinate dysfunction at some point in their lives.
Causes of Turbinate Dysfunction
Allergic rhinitis is a leading cause of turbinate dysfunction. Swelling (hypertrophy) of the inferior turbinate can occur as a result of:
- Allergies
- Changes in temperature
- Environmental irritants (chemicals)
- Upper respiratory infection (URI)
- Allergic rhinitis
- Vasomotor rhinitis
- Drugs or hormones
Oftentimes, swelling is reversible. Persistent swelling, however, can become chronic and results in turbinate hypertrophy.
Symptoms of Turbinate Hypertrophy
When the inferior turbinates become inflamed and enlarged, they can cause the following symptoms:
- Total nasal obstruction (congestion, trouble breathing)
- Mild congestion
- Rhinorrhea (runny nose)
- Post nasal drip
- Snoring
- Chronic nosebleeds (sometimes a result of a deviated septum)
- Chronic sinus infections
How Our Allergy Doctors Treat Turbinate Hypertrophy
Our allergy doctors use the Turbinator Wand (see video) as a surgical technique to reduce the size of the inferior turbinate while preserving its natural lining to preserve function.
The procedure to reduce swelling of the inferior turbinate is minimally invasive and performed in the office. The patient’s nose is numbed so the patient is comfortable without the need for IV or sedation. Patients can drive themselves to the office and drive themselves home afterward.
What to Expect After Turbinate Hypertrophy Treatment
Patients should expect a degree of stuffiness and congestion during the healing period but results have proven a reduction in runny nose, post nasal drip, nasal congestion, nosebleeds, infections, and snoring.
Q: Will this procedure cure my allergies?
A: Patients experience a varied level of relief from symptoms, ranging from decreased symptoms to “it changed my life.”
Q: Will I still need allergy medicines after the procedure?
A: Your need for medicines may be less than before the procedure and, in many cases, not needed at all.
Q: Will I be awake during the procedure?
A: Yes. Your allergy doctor will numb you and ensure your complete comfort during the turbinate hypertrophy procedure.
Q: Will I need an IV?
A: No. Because of the thorough numbing process, the procedure is completely comfortable with the convenience of being awake.
Q: Will I need a ride home?
A: No. You may drive yourself to and from the office-based procedure. Sometimes, at the patient’s request, we admit an oral sedative which would require that you get a ride home.
